
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Guideline/Fact Sheet
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae Jin Kim, Hyun Min Kim, Jung Hae Ko, Nam Hoon Kim, Chong Hwa Kim, Jeeyun Ahn, Tae Jung Oh, Soo-Kyung Kim, Jaehyun Kim, Eugene Han, Sang-Man Jin, Won Suk Choi, Min Kyong Moon, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2023;47(5):575-594. Published online September 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0282
- 5,121 View
- 638 Download
- 8 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
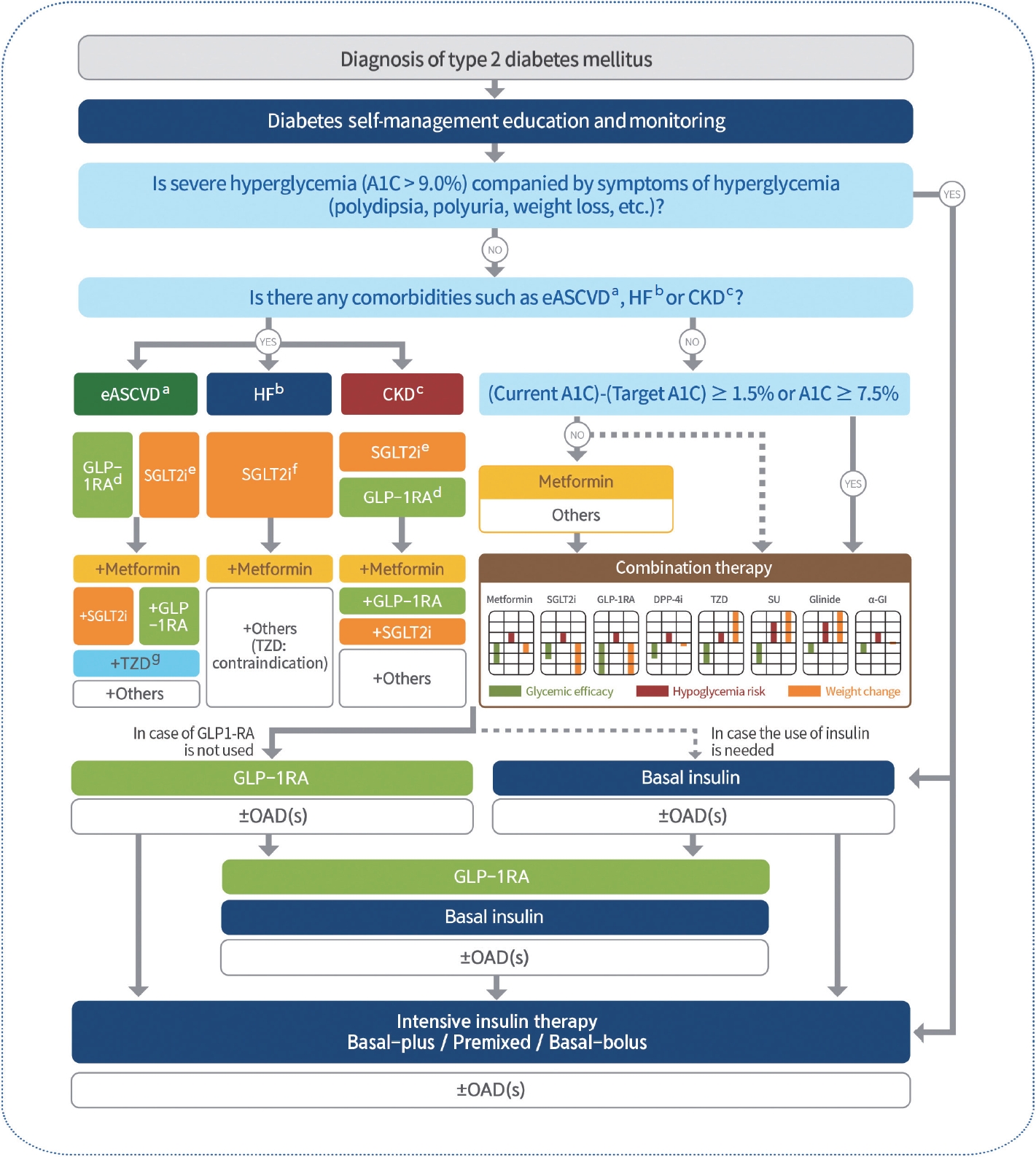
ePub - In May 2023, the Committee of Clinical Practice Guidelines of the Korean Diabetes Association published the revised clinical practice guidelines for Korean adults with diabetes and prediabetes. We incorporated the latest clinical research findings through a comprehensive systematic literature review and applied them in a manner suitable for the Korean population. These guidelines are designed for all healthcare providers nationwide, including physicians, diabetes experts, and certified diabetes educators who manage patients with diabetes or individuals at risk of developing diabetes. Based on recent changes in international guidelines and the results of a Korean epidemiological study, the recommended age for diabetes screening has been lowered. In collaboration with the relevant Korean medical societies, recently revised guidelines for managing hypertension and dyslipidemia in patients with diabetes have been incorporated into this guideline. An abridgment containing practical information on patient education and systematic management in the clinic was published separately.
-
Citations
Citations to this article as recorded by- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Letter by In-Kyung Jeong Regarding Article, Trends in Prevalence of Hypertriglyceridemia and Related Factors in Korean Adults: A Serial Cross-Sectional Study
In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2024; 13(1): 80. CrossRef - Association between cardiovascular disease risk and incident type 2 diabetes mellitus in individuals with prediabetes: A retrospective cohort study
Myung Jin Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee
Diabetes Research and Clinical Practice.2024; 208: 111125. CrossRef - Korea Hypertension Fact Sheet 2023: analysis of nationwide population-based data with a particular focus on hypertension in special populations
Hyeon Chang Kim, Hokyou Lee, Hyeok-Hee Lee, Dasom Son, Minsung Cho, Sojung Shin, Yeeun Seo, Eun-Jin kim, Song Vogue Ahn, Sun Ha Jee, Sungha Park, Hae-Young Lee, Min Ho Shin, Sang-Hyun Ihm, Seung Won Lee, Jong Ku Park, Il Suh, Tae-Yong Lee
Clinical Hypertension.2024;[Epub] CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Effect of Adding Apolipoprotein B Testing on the Prevalence of Dyslipidemia and Risk of Cardiovascular Disease in the Korean Adult Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Metabolites.2024; 14(3): 169. CrossRef - A self-powered and supercapacitive microneedle continuous glucose monitoring system with a wide range of glucose detection capabilities
Hye-Jun Kil, Jang Hyeon Kim, Kanghae Lee, Tae-Uk Kang, Ju-Hyun Yoo, Yong-ho Lee, Jin-Woo Park
Biosensors and Bioelectronics.2024; 257: 116297. CrossRef - Cardiorenal outcomes and mortality after sodium‐glucose cotransporter‐2 inhibitor initiation in type 2 diabetes patients with percutaneous coronary intervention history
Jin Hwa Kim, Young Sang Lyu, BongSeong Kim, Mee Kyung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Recommendations for Pharmacological Treatment of Type 2 Diabetes
Junghyun Noh
The Journal of Korean Diabetes.2023; 24(3): 127. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - A 33-Year-Old Man Presented with Abdominal Pain and Vomiting Starting a Day Ago
Jong Han Choi
The Korean Journal of Medicine.2023; 98(6): 289. CrossRef - Comorbidity Patterns and Management in Inpatients with Endocrine Diseases by Age Groups in South Korea: Nationwide Data
Sung-Soo Kim, Hun-Sung Kim
Journal of Personalized Medicine.2023; 14(1): 42. CrossRef
- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
- Guideline/Fact Sheet
- Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
- Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon, on Behalf of the Committee of Clinical Practice Guideline of Korean Diabetes Association
- Diabetes Metab J. 2022;46(6):819-826. Published online November 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0364
- 4,297 View
- 270 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
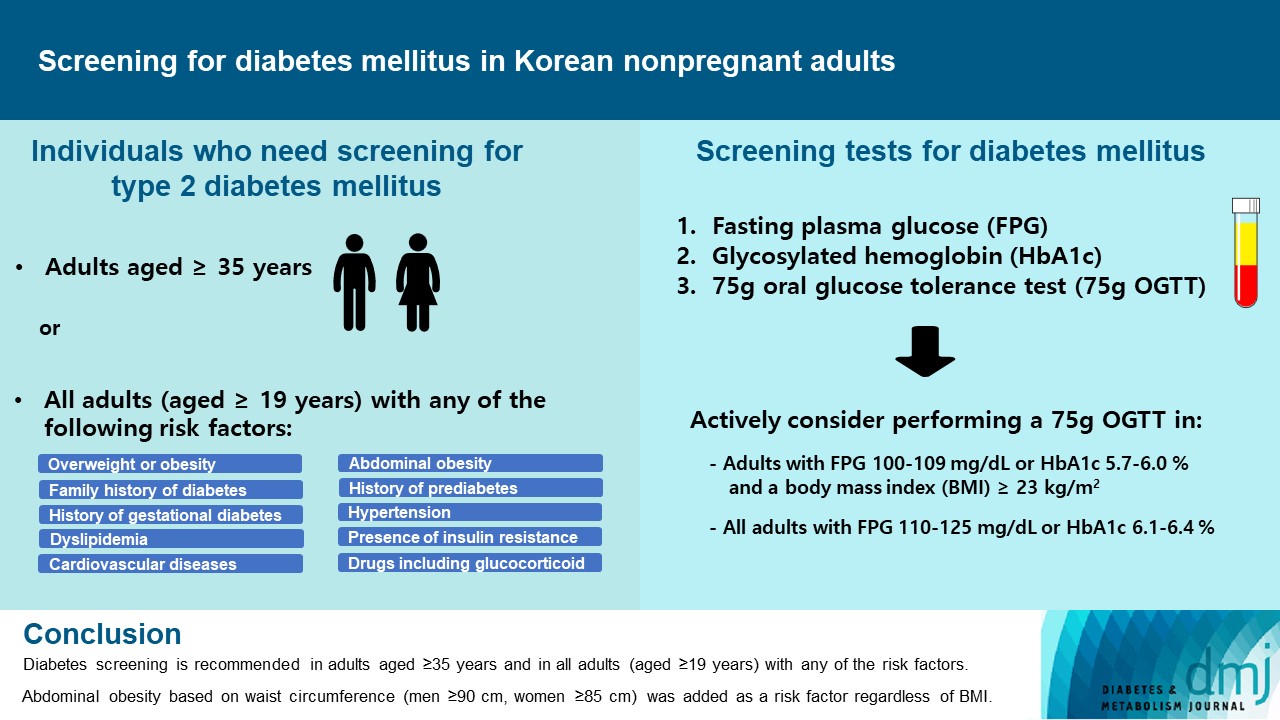
ePub - Diabetes screening serves to identify individuals at high-risk for diabetes who have not yet developed symptoms and to diagnose diabetes at an early stage. Globally, the prevalence of diabetes is rapidly increasing. Furthermore, obesity and/or abdominal obesity, which are major risk factors for type 2 diabetes mellitus (T2DM), are progressively increasing, particularly among young adults. Many patients with T2DM are asymptomatic and can accompany various complications at the time of diagnosis, as well as chronic complications develop as the duration of diabetes increases. Thus, proper screening and early diagnosis are essential for diabetes care. Based on reports on the changing epidemiology of diabetes and obesity in Korea, as well as growing evidence from new national cohort studies on diabetes screening, the Korean Diabetes Association has updated its clinical practice recommendations regarding T2DM screening. Diabetes screening is now recommended in adults aged ≥35 years regardless of the presence of risk factors, and in all adults (aged ≥19) with any of the risk factors. Abdominal obesity based on waist circumference (men ≥90 cm, women ≥85 cm) was added to the list of risk factors.
-
Citations
Citations to this article as recorded by- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
Mid-Eum Moon, Dong Hyuk Jung, Seok-Jae Heo, Byoungjin Park, Yong Jae Lee
Antioxidants.2024; 13(1): 107. CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Cumulative muscle strength and risk of diabetes: A prospective cohort study with mediation analysis
Shanhu Qiu, Xue Cai, Yan Liang, Wenji Chen, Duolao Wang, Zilin Sun, Bo Xie, Tongzhi Wu
Diabetes Research and Clinical Practice.2023; 197: 110562. CrossRef - Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef
- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
- Complications
- Influence of Glucose Fluctuation on Peripheral Nerve Damage in Streptozotocin-Induced Diabetic Rats
- Yu Ji Kim, Na Young Lee, Kyung Ae Lee, Tae Sun Park, Heung Yong Jin
- Diabetes Metab J. 2022;46(1):117-128. Published online September 9, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0275
- 5,231 View
- 179 Download
- 4 Web of Science
- 4 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 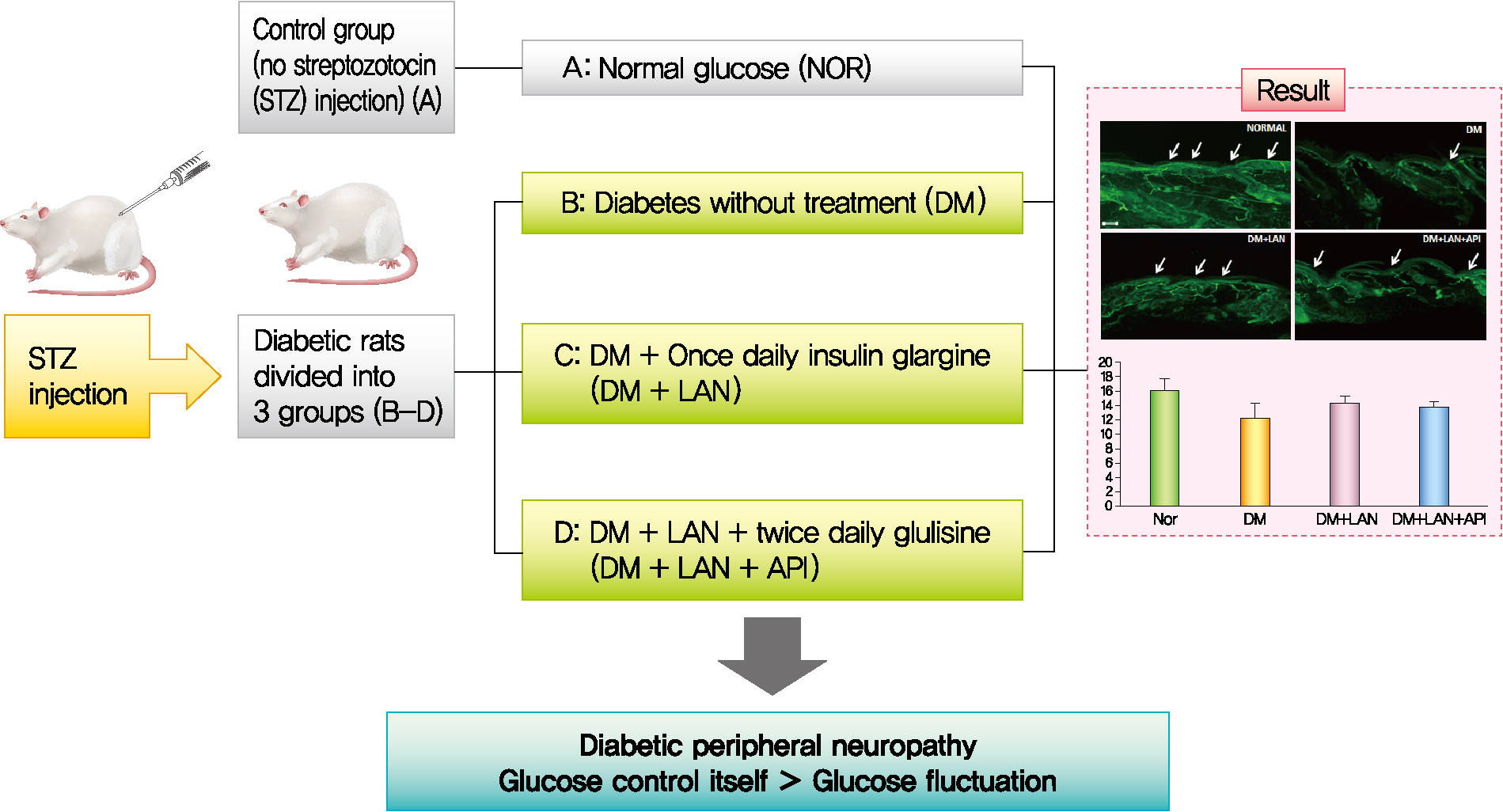
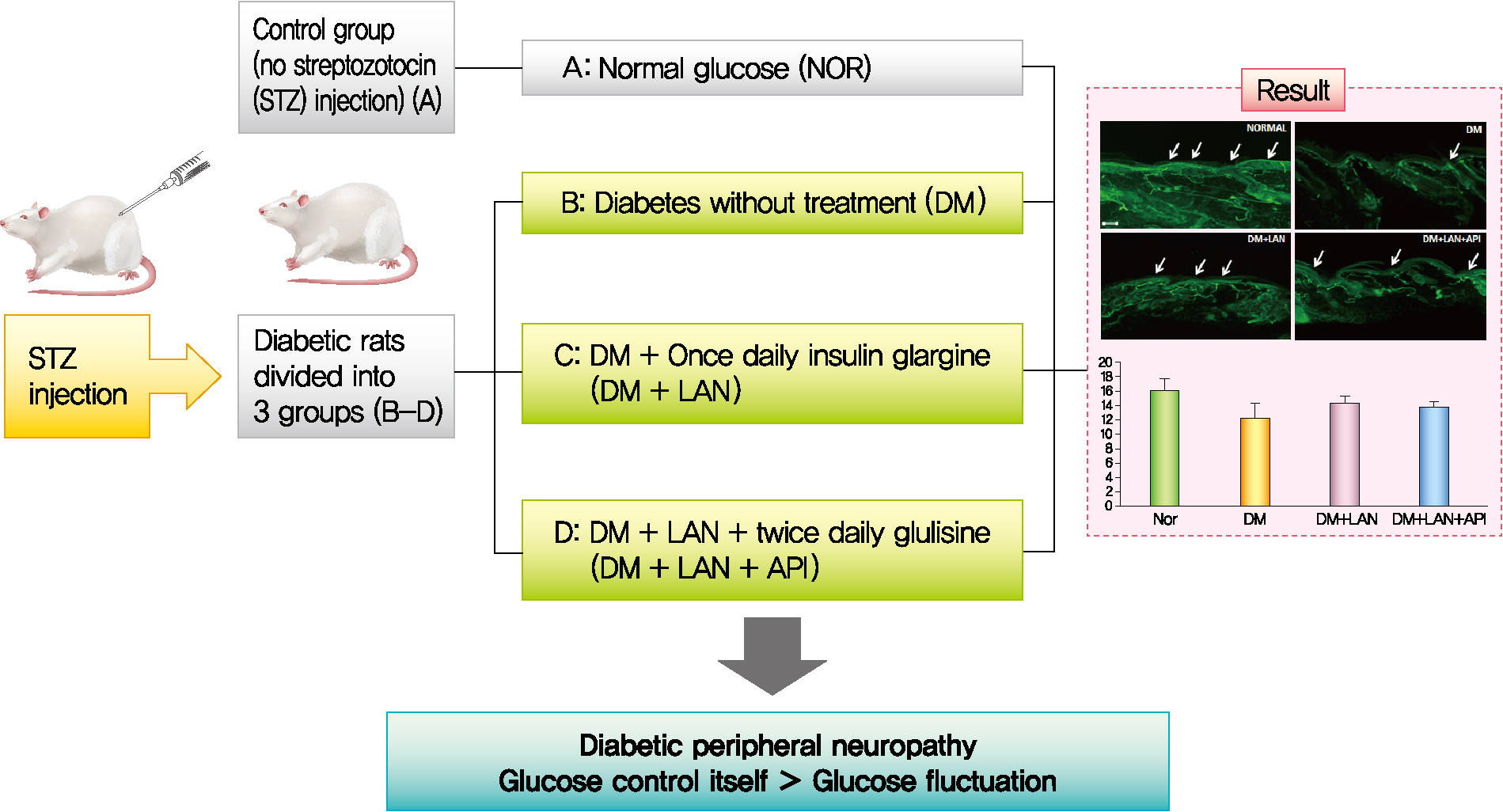
- Background
It is unclear whether glycemic variability (GV) is a risk factor for diabetic peripheral neuropathy (DPN), and whether control of GV is beneficial for DPN. The purpose of this study was to investigate the effect of GV on peripheral nerve damage by inducing glucose fluctuation in streptozotocin-induced diabetic rats.
Methods
Rats were divided into four groups: normal (normal glucose group [NOR]), diabetes without treatment (sustained severe hyperglycemia group; diabetes mellitus [DM]), diabetes+once daily insulin glargine (stable hyperglycemia group; DM+LAN), and diabetes+once daily insulin glargine with twice daily insulin glulisine (unstable glucose fluctuation group; DM+Lantus [LAN]+Apidra [API]). We measured anti-oxidant enzyme levels and behavioral responses against tactile, thermal, and pressure stimuli in the plasma of rats. We also performed a quantitative comparison of cutaneous and sciatic nerves according to glucose fluctuation.
Results
At week 24, intraepidermal nerve fiber density was less reduced in the insulin-administered groups compared to the DM group (P<0.05); however, a significant difference was not observed between the DM+LAN and DM+LAN+API groups irrespective of glucose fluctuation (P>0.05; 16.2±1.6, 12.4±2.0, 14.3±0.9, and 13.9±0.6 for NOR, DM, DM+LAN, and DM+LAN+API, respectively). The DM group exhibited significantly decreased glutathione levels compared to the insulin-administered groups (2.64±0.10 μmol/mL, DM+LAN; 1.93±0.0 μmol/mL, DM+LAN+API vs. 1.25±0.04 μmol/mL, DM; P<0.05).
Conclusion
Our study suggests that glucose control itself is more important than glucose fluctuation in the prevention of peripheral nerve damage, and intra-day glucose fluctuation has a limited effect on the progression of peripheral neuropathy in rats with diabetes. -
Citations
Citations to this article as recorded by- Glucose Fluctuation Inhibits Nrf2 Signaling Pathway in Hippocampal Tissues and Exacerbates Cognitive Impairment in Streptozotocin-Induced Diabetic Rats
Haiyan Chi, Yujing Sun, Peng Lin, Junyu Zhou, Jinbiao Zhang, Yachao Yang, Yun Qiao, Deshan Liu, Eusebio Chiefari
Journal of Diabetes Research.2024; 2024: 1. CrossRef - Artesunate Inhibits Apoptosis and Promotes Survival in Schwann Cells via the PI3K/AKT/mTOR Axis in Diabetic Peripheral Neuropathy
Xin Zhang, Zhifang Liang, Ying Zhou, Fang Wang, Shan Wei, Bing Tan, Yujie Guo
Biological and Pharmaceutical Bulletin.2023; 46(6): 764. CrossRef - The Potential of Glucose Treatment to Reduce Reactive Oxygen Species Production and Apoptosis of Inflamed Neural Cells In Vitro
Juin-Hong Cherng, Shu-Jen Chang, Hsin-Da Tsai, Chung-Fang Chun, Gang-Yi Fan, Kenneth Dean Reeves, King Hei Stanley Lam, Yung-Tsan Wu
Biomedicines.2023; 11(7): 1837. CrossRef - Relationship between acute glucose variability and cognitive decline in type 2 diabetes: A systematic review and meta-analysis
Haiyan Chi, Min Song, Jinbiao Zhang, Junyu Zhou, Deshan Liu, Victor Manuel Mendoza-Nuñez
PLOS ONE.2023; 18(9): e0289782. CrossRef
- Glucose Fluctuation Inhibits Nrf2 Signaling Pathway in Hippocampal Tissues and Exacerbates Cognitive Impairment in Streptozotocin-Induced Diabetic Rats
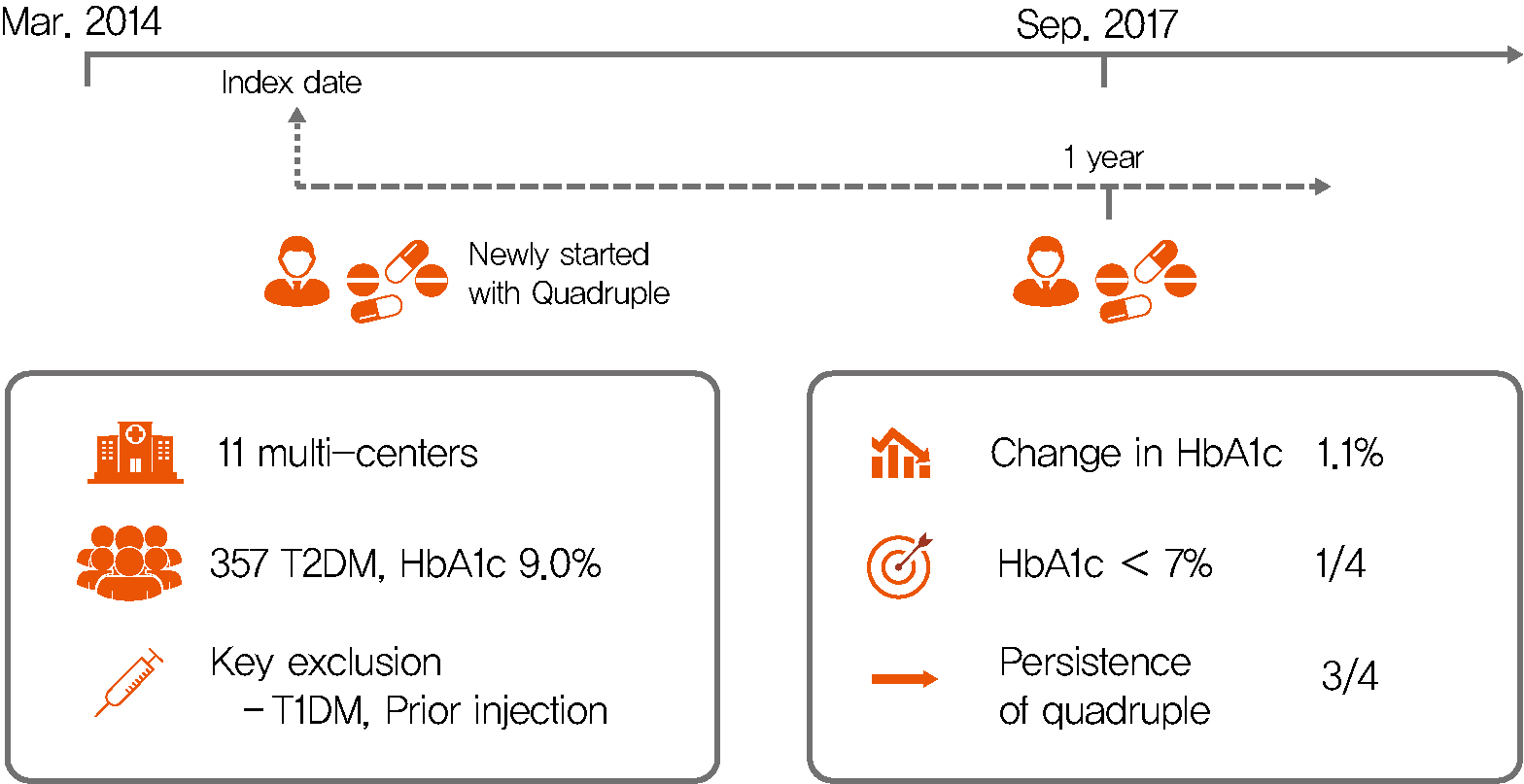
- Drug/Regimen
- Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
- Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Kim, Hye Soon Kim, Il Seong Nam-Goong, Eun Sook Kim, Jin Ook Chung, Dong-Hyeok Cho, Chang Won Lee, Young Il Kim, Dong Jin Chung, Kyu Chang Won, In Joo Kim, Tae Sun Park, Duk Kyu Kim, Hosang Shon
- Diabetes Metab J. 2021;45(5):675-683. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0107
- 35,380 View
- 367 Download
- 9 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 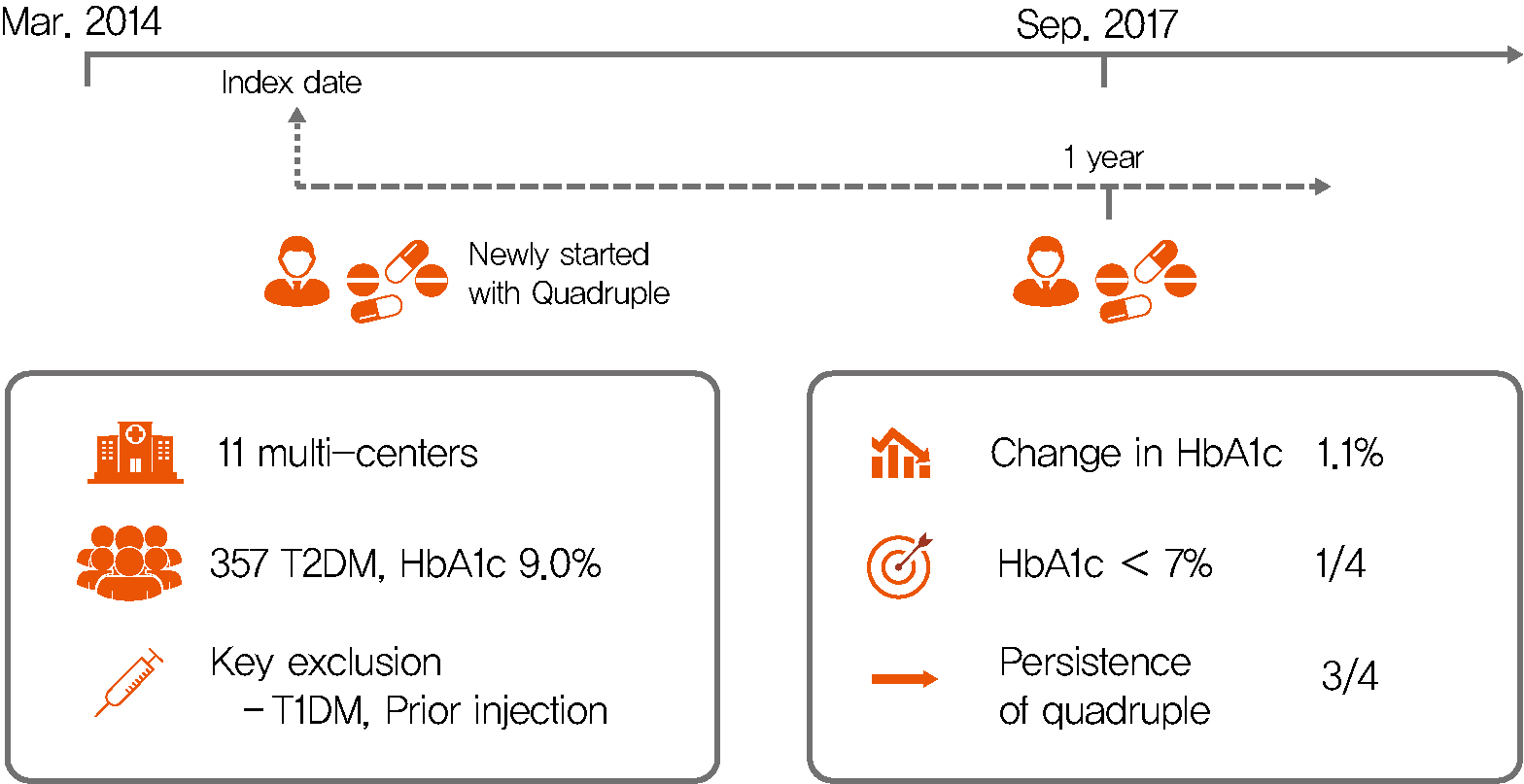
Background Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%;
P <0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P <0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.Conclusion This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
-
Citations
Citations to this article as recorded by- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
Rita Oliveira, Matilde Monteiro-Soares, José Pedro Guerreiro, Rúben Pereira, António Teixeira-Rodrigues
Pharmacy.2024; 12(1): 18. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef
- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
- Complications
- Effect of Empagliflozin, a Selective Sodium-Glucose Cotransporter 2 Inhibitor, on Kidney and Peripheral Nerves in Streptozotocin-Induced Diabetic Rats
- Kyung Ae Lee, Heung Yong Jin, Na Young Lee, Yu Ji Kim, Tae Sun Park
- Diabetes Metab J. 2018;42(4):338-342. Published online April 25, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0095
- 3,996 View
- 64 Download
- 17 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The effect of sodium-glucose cotransporter 2 inhibitors on peripheral nerves and kidneys in diabetes mellitus (DM) remains unexplored. Therefore, this study aimed to explore the effect of empagliflozin in diabetic rats. DM in rats was induced by streptozotocin injection, and diabetic rats were treated with empagliflozin 3 or 10 mg/kg. Following 24-week treatment, response thresholds to four different stimuli were tested and found to be lower in diabetic rats than in normal rats. Empagliflozin significantly prevented hypersensitivity (
P <0.05) and the loss of skin intraepidermal nerve fibers, and mesangial matrix expansion in diabetic rats. Results of this study demonstrate the potential therapeutic effects of empagliflozin for the treatment of diabetic peripheral neuropathy and nephropathy.-
Citations
Citations to this article as recorded by- Effect of empagliflozin in peripheral diabetic neuropathy of patients with type 2 diabetes mellitus
Sahar Mohamed El-Haggar, Yasser Mostafa Hafez, Amira Mohamed El Sharkawy, Maha Khalifa
Medicina Clínica.2024;[Epub] CrossRef - A Review of Recent Pharmacological Advances in the Management of Diabetes-Associated Peripheral Neuropathy
Osman Syed, Predrag Jancic, Nebojsa Nick Knezevic
Pharmaceuticals.2023; 16(6): 801. CrossRef - Renal intrinsic cells remodeling in diabetic kidney disease and the regulatory effects of SGLT2 Inhibitors
Wenwen Guo, Han Li, Yixuan Li, Wen Kong
Biomedicine & Pharmacotherapy.2023; 165: 115025. CrossRef - A systematic review on renal effects of SGLT2 inhibitors in rodent models of diabetic nephropathy
Aqsa Ashfaq, Myriam Meineck, Andrea Pautz, Ebru Arioglu-Inan, Julia Weinmann-Menke, Martin C. Michel
Pharmacology & Therapeutics.2023; 249: 108503. CrossRef - The impact of canagliflozin on the risk of neuropathy events: A post-hoc exploratory analysis of the CREDENCE trial
Jinlan Liao, Amy Kang, Chao Xia, Tamara Young, Gian Luca Di Tanna, Clare Arnott, Carol Pollock, Arun V. Krishnan, Rajiv Agarwal, George Bakris, David M. Charytan, Dick de Zeeuw, Hiddo J.L. Heerspink, Adeera Levin, Bruce Neal, David C. Wheeler, Hong Zhang,
Diabetes & Metabolism.2022; 48(4): 101331. CrossRef - Sodium Glucose Cotransporter-2 Inhibitor Protects Against Diabetic Neuropathy and Nephropathy in Modestly Controlled Type 2 Diabetes: Follow-Up Study
Fukashi Ishibashi, Aiko Kosaka, Mitra Tavakoli
Frontiers in Endocrinology.2022;[Epub] CrossRef - Protective effect of empagliflozin on gentamicin-induced acute renal injury via regulation of SIRT1/NF-κB signaling pathway
Sandy R. Botros, Asmaa I. Matouk, Aliaa Anter, Mohamed M.A. Khalifa, Gehan H. Heeba
Environmental Toxicology and Pharmacology.2022; 94: 103907. CrossRef - Empagliflozin mitigates type 2 diabetes-associated peripheral neuropathy: a glucose-independent effect through AMPK signaling
Noha F. Abdelkader, Marawan A. Elbaset, Passant E. Moustafa, Sherehan M. Ibrahim
Archives of Pharmacal Research.2022; 45(7): 475. CrossRef - Pathogenesis and Treatment of Diabetic Peripheral Neuropathy
Seon Mee Kang
The Journal of Korean Diabetes.2022; 23(4): 222. CrossRef - Empagliflozin and neohesperidin protect against methotrexate-induced renal toxicity via suppression of oxidative stress and inflammation in male rats
Adel T. Osman, Souty M.Z. Sharkawi, Mohamed I.A. Hassan, Amira M. Abo-youssef, Ramadan A.M. Hemeida
Food and Chemical Toxicology.2021; 155: 112406. CrossRef - Effect of exenatide on peripheral nerve excitability in type 2 diabetes
Tushar Issar, Natalie C.G. Kwai, Ann M. Poynten, Ria Arnold, Kerry-Lee Milner, Arun V. Krishnan
Clinical Neurophysiology.2021; 132(10): 2532. CrossRef - Effectiveness of Empagliflozin With Vitamin D Supplementation in Peripheral Neuropathy in Type 2 Diabetic Patients
Sanjana Mehta, Parminder Nain, Bimal K Agrawal, Rajinder P Singh, Jaspreet Kaur, Sabyasachi Maity, Aniruddha Bhattarcharjee, Jagannadha Peela, Shreya Nauhria, Samal Nauhria
Cureus.2021;[Epub] CrossRef - Targeting oxidative stress, proinflammatory cytokines, apoptosis and toll like receptor 4 by empagliflozin to ameliorate bleomycin-induced lung fibrosis
Ahmed M. Kabel, Remon S. Estfanous, Majed M. Alrobaian
Respiratory Physiology & Neurobiology.2020; 273: 103316. CrossRef - Empagliflozin reduces high glucose-induced oxidative stress and miR-21-dependent TRAF3IP2 induction and RECK suppression, and inhibits human renal proximal tubular epithelial cell migration and epithelial-to-mesenchymal transition
Nitin A. Das, Andrea J. Carpenter, Anthony Belenchia, Annayya R. Aroor, Makoto Noda, Ulrich Siebenlist, Bysani Chandrasekar, Vincent G. DeMarco
Cellular Signalling.2020; 68: 109506. CrossRef - Differential Effects of Empagliflozin on Microvascular Complications in Murine Models of Type 1 and Type 2 Diabetes
Stephanie A. Eid, Phillipe D. O’Brien, Lucy M. Hinder, John M. Hayes, Faye E. Mendelson, Hongyu Zhang, Lixia Zeng, Katharina Kretzler, Samanthi Narayanan, Steven F. Abcouwer, Frank C. Brosius, Subramaniam Pennathur, Masha G. Savelieff, Eva L. Feldman
Biology.2020; 9(11): 347. CrossRef - Pre-treatment with Empagliflozin ameliorates Cisplatin induced acute kidney injury by suppressing apoptosis
Maaly A. Abd Elmaaboud, Ahmed M. Kabel, Mohamed Elrashidy
Journal of Applied Biomedicine.2019; 17(1): 90. CrossRef - Effects of ticagrelor, empagliflozin and tamoxifen against experimentally-induced vascular reactivity defects in rats in vivo and in vitro
Yasmin Moustafa Ahmed, Basim Anwar Shehata Messiha, Mahmoud El-Sayed El-Daly, Ali Ahmed Abo-Saif
Pharmacological Reports.2019; 71(6): 1034. CrossRef - SGLT2 inhibition with empagliflozin attenuates myocardial oxidative stress and fibrosis in diabetic mice heart
Chenguang Li, Jie Zhang, Mei Xue, Xiaoyu Li, Fei Han, Xiangyang Liu, Linxin Xu, Yunhong Lu, Ying Cheng, Ting Li, Xiaochen Yu, Bei Sun, Liming Chen
Cardiovascular Diabetology.2019;[Epub] CrossRef - Empagliflozin Contributes to Polyuria via Regulation of Sodium Transporters and Water Channels in Diabetic Rat Kidneys
Sungjin Chung, Soojeong Kim, Mina Son, Minyoung Kim, Eun Sil Koh, Seok Joon Shin, Seung-Hyun Ko, Ho-Shik Kim
Frontiers in Physiology.2019;[Epub] CrossRef
- Effect of empagliflozin in peripheral diabetic neuropathy of patients with type 2 diabetes mellitus
- Complication
- Morphologic Comparison of Peripheral Nerves in Adipocyte Tissue from
db/db Diabetic versus Normal Mice - Kyung Ae Lee, Na Young Lee, Tae Sun Park, Heung Yong Jin
- Diabetes Metab J. 2018;42(2):169-172. Published online March 21, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.169
- 3,398 View
- 43 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Present study investigated the morphologic changes of autonomic nerves in the adipose tissue in diabetic animal model. Male obese type 2 diabetic
db/db mice and age matched non-diabeticdb/m control mice were used. Epididymal adipose tissue from diabeticdb/db mice with that from control heterozygousdb/m mice was compared using confocal microscopy-based method to visualize intact whole adipose tissue. Immunohistochemistry with tyrosine hydroxylase for sympathetic (SP), choline acetyltransferase for parasympathetic (PSP), and protein gene product 9.5 (PGP 9.5) for whole autonomic nerves was performed. The quantity of immunostained portion of SP, PSP, and PGP 9.5 stained nerve fibers showed decreased trend in diabetic group; however, the ratio of SP/PSP of adipose tissue was higher in diabetic group compared with control group as follows (0.70±0.30 vs. 0.95±0.25,P <0.05; normal vs. diabetic, respectively). Both SP and PSP nerve fibers were observed in white adipose tissue and PSP nerve fibers were suggested as more decreased in diabetes based on our observation.
- The Relationship between Anemia and the Initiation of Dialysis in Patients with Type 2 Diabetic Nephropathy
- Sun Hee Kim, Kyung Ae Lee, Heung Yong Jin, Hong Sun Baek, Tae Sun Park
- Diabetes Metab J. 2015;39(3):240-246. Published online April 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.240
- 3,677 View
- 32 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Anemia is associated with various poor clinical outcomes in chronic kidney disease patients. The aim of this study was to investigate the relationship between anemia and the initiation degree and time of dialysis in type 2 diabetic nephropathy patients.
Methods This observational retrospective study included 130 type 2 diabetic nephropathy patients in Korea. The existence of anemia, the degree and time of dialysis initiation were reviewed. Clinical characteristics and variables were also compared.
Results The levels of hemoglobin and serum creatinine were significantly correlated with the dialysis initiation (
P <0.05) during the 10-year follow-up period. Patients with anemia showed rapid decline of renal function, causing significantly more dialysis initiation (54.1% vs. 5.4%,P <0.05) compare to the patients without anemia. Average time to initiate dialysis in patients with anemia was 45.1 months (range, 8.0 to 115.8 months), which was significantly faster than that (68.3 months [range, 23.3 to 108.8 months]) in patients without anemia (P <0.01). The risk to dialysis initiation was significantly increased in patients with anemia compared to the patients without anemia (adjusted hazard ratio, 8.1; 95% confidence interval, 2.4 to 27.0;P <0.05).Conclusion Anemia is associated with rapid decline of renal dysfunction and faster initiation of dialysis in diabetic nephropathy patients. Therefore, clinicians should pay an earlier attention to anemia during the management of diabetes.
-
Citations
Citations to this article as recorded by- Microalbuminuria as the Tip of Iceberg in Type 2 Diabetes Mellitus: Prevalence, Risk Factors, and Associated Diabetic Complications
Sohaib Asghar, Shoaib Asghar, Tayyab Mahmood, Syed Muhammad Hassan Bukhari, Muhammad Habib Mumtaz, Ali Rasheed
Cureus.2023;[Epub] CrossRef - The Association between Serum Hemoglobin and Renal Prognosis of IgA Nephropathy
Tae Ryom Oh, Su Hyun Song, Hong Sang Choi, Chang Seong Kim, Seung Hyeok Han, Kyung Pyo Kang, Young Joo Kwon, Soo Wan Kim, Seong Kwon Ma, Eun Hui Bae
Journal of Clinical Medicine.2021; 10(2): 363. CrossRef - Prevalence of anemia in diabetic adult outpatients in Northeast Ethiopia
Temesgen Fiseha, Aderaw Adamu, Melkam Tesfaye, Angesom Gebreweld, Jennifer A. Hirst
PLOS ONE.2019; 14(9): e0222111. CrossRef - Targeted Clinical Metabolite Profiling Platform for the Stratification of Diabetic Patients
Ahonen, Jäntti, Suvitaival, Theilade, Risz, Kostiainen, Rossing, Orešič, Hyötyläinen
Metabolites.2019; 9(9): 184. CrossRef - Effect of high density lipoprotein cholesterol on the relationship of serum iron and hemoglobin with kidney function in diabetes
Ashley N. Williams, Baqiyyah N. Conway
Journal of Diabetes and its Complications.2017; 31(6): 958. CrossRef
- Microalbuminuria as the Tip of Iceberg in Type 2 Diabetes Mellitus: Prevalence, Risk Factors, and Associated Diabetic Complications
- Relationship between the Korean Version Survey of the Autonomic Symptoms Score and Cardiac Autonomic Neuropathy Parameters in Patients with Diabetic Peripheral Neuropathy
- Sun Hee Kim, Kyung Ae Lee, Heung Yong Jin, Hong Sun Baek, Tae Sun Park
- Diabetes Metab J. 2014;38(5):349-355. Published online October 17, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.5.349
- 5,186 View
- 51 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The Survey of Autonomic Symptom (SAS) scale was reported as an easy instrument to assess the autonomic symptoms in patients with early diabetic neuropathy. In this study, we investigated the relationship between the SAS scale and the parameters of cardiac autonomic neuropathy (CAN) in Korean patients with diabetic peripheral neuropathy (DPN).
Methods The SAS scale was tested in 30 healthy controls and 73 patients with DPN at Chonbuk National University Hospital, in Korea. The SAS score was compared to the parameters of the CAN test and the total symptom score (TSS) for DPN in patients with DPN.
Results The SAS symptom score and total impact score were increased in patients with DPN compared to the control group (
P =0.01), particularly in sudomotor dysfunction (P =0.01), and vasomotor dysfunction (P =0.01). The SAS score was increased in patients with CAN compared to patients without CAN (P <0.05). Among the diverse CAN parameters, the valsalva ratio and postural hypotension were associated with the SAS score (P <0.05). However, there was no association between the SAS scale and TSS for DPN, and TSS for DPN did not differ between patients with and without CAN.Conclusion SAS is a simple instrument that can be used to assess autonomic symptoms in patients with diabetes and can be used as a screening tool for autonomic neuropathy, particularly for CAN.
-
Citations
Citations to this article as recorded by- Autonomic neuropathic symptoms in patients with diabetes: practical tools for screening in daily routine
Ana Raquel Souza de Azevedo Vieira, Lara Benigno Porto-Dantas, Flaviene Alves do Prado Romani, Patrícia Souza Carvalho, Rodica Pop-Busui, Hermelinda Cordeiro Pedrosa
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Symptomatic diabetic autonomic neuropathy in type 1 diabetes (T1D): Findings from the T1D exchange
Kara Mizokami-Stout, Ryan Bailey, Lynn Ang, Grazia Aleppo, Carol J. Levy, Michael R. Rickels, Viral N. Shah, Sarit Polsky, Bryce Nelson, Anders L. Carlson, Francesco Vendrame, Rodica Pop-Busui
Journal of Diabetes and its Complications.2022; 36(5): 108148. CrossRef - Clinical Assessment Scales in Autonomic Nervous System Disorders
Eun Bin Cho, Ki-Jong Park
Journal of the Korean Neurological Association.2021; 39(2 Suppl): 60. CrossRef - Peripheral Nerve Conduction And Sympathetic Skin Response Are Reliable Methods to Detect Diabetic Cardiac Autonomic Neuropathy
Xiaopu Lin, Chuna Chen, Yingshan Liu, Yu Peng, Zhenguo Chen, Haishan Huang, Lingling Xu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Predictive model to identify the risk of losing protective sensibility of the foot in patients with diabetes mellitus
Esther Chicharro‐Luna, Francisco José Pomares‐Gómez, Ana Belen Ortega‐Ávila, Ana Marchena‐Rodríguez, José Francisco Javier Blanquer‐Gregori, Emmanuel Navarro‐Flores
International Wound Journal.2020; 17(1): 220. CrossRef - The hemodynamic and pain impact of peripheral nerve block versus spinal anesthesia in diabetic patients undergoing diabetic foot surgery
Hou Yee Lai, Li Lian Foo, Siu Min Lim, Chen Fei Yong, Pui San Loh, Sook Hui Chaw, Mohd Shahnaz Hasan, Chew Yin Wang
Clinical Autonomic Research.2020; 30(1): 53. CrossRef - Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
Vincenza Spallone
Diabetes & Metabolism Journal.2019; 43(1): 3. CrossRef - Validation of the Composite Autonomic Symptom Score 31 (COMPASS 31) for the assessment of symptoms of autonomic neuropathy in people with diabetes
C. Greco, F. Di Gennaro, C. D'Amato, R. Morganti, D. Corradini, A. Sun, S. Longo, D. Lauro, G. Pierangeli, P. Cortelli, V. Spallone
Diabetic Medicine.2017; 34(6): 834. CrossRef - Cardiovascular Autonomic Dysfunction Predicts Diabetic Foot Ulcers in Patients With Type 2 Diabetes Without Diabetic Polyneuropathy
Jae-Seung Yun, Seon-Ah Cha, Tae-Seok Lim, Eun-Young Lee, Ki-Ho Song, Yu-Bae Ahn, Ki-Dong Yoo, Joon-Sung Kim, Yong-Moon Park, Seung-Hyun Ko
Medicine.2016; 95(12): e3128. CrossRef - Retinal Neurodegeneration Associated With Peripheral Nerve Conduction and Autonomic Nerve Function in Diabetic Patients
Kiyoung Kim, Seung-Young Yu, Hyung Woo Kwak, Eung Suk Kim
American Journal of Ophthalmology.2016; 170: 15. CrossRef - Screening of Autonomic Neuropathy in Patients with Type 2 Diabetes
Bo Kyung Koo
Diabetes & Metabolism Journal.2014; 38(5): 346. CrossRef
- Autonomic neuropathic symptoms in patients with diabetes: practical tools for screening in daily routine
- Effect of Granulocyte Colony-Stimulating Factor on the Peripheral Nerves in Streptozotocin-Induced Diabetic Rat
- Kyung Ae Lee, Kyung Taek Park, Hea Min Yu, Heung Yong Jin, Hong Sun Baek, Tae Sun Park
- Diabetes Metab J. 2013;37(4):286-290. Published online August 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.4.286
- 3,220 View
- 26 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader There are controversial reports about the effect of granulocyte colony-stimulating factor (G-CSF) in peripheral nerve protection. Therefore, the present study aimed to investigate the effect of G-CSF on peripheral nerves in streptozotocin (STZ) induced diabetic rats. After STZ or vehicle injection, rats were divided into five groups (
n =6) as follows: normal+vehicle, normal+G-CSF (50 µg/kg for 5 days), diabetes mellitus (DM)+vehicle, DM+G-CSF (50 µg/kg for 5 days), and DM+G-CSF extension (50 µg/kg for 5 days and followed by two injections per week up to 24 weeks). Our results showed that the current perception threshold was not significantly different among experimental groups. G-CSF treatment inhibited the loss of cutaneous nerves and gastric mucosal small nerve fibers in morphometric comparison, but statistical significance was not observed. The present results demonstrated that G-CSF has no harmful but minimal beneficial effects with respect to peripheral nerve preservation in diabetic rats.-
Citations
Citations to this article as recorded by- Colony stimulating factors in the nervous system
Violeta Chitu, Fabrizio Biundo, E. Richard Stanley
Seminars in Immunology.2021; 54: 101511. CrossRef - Non-glucose risk factors in the pathogenesis of diabetic peripheral neuropathy
Kyung Ae Lee, Tae Sun Park, Heung Yong Jin
Endocrine.2020; 70(3): 465. CrossRef - Two to Tango: Dialogue between Adaptive and Innate Immunity in Type 1 Diabetes
Lin Sun, Shugang Xi, Guangyu He, Zhuo Li, Xiaokun Gang, Chenglin Sun, Weiying Guo, Guixia Wang
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Transplantation of human mobilized mononuclear cells improved diabetic neuropathy
Se Hee Min, Jung Hee Kim, Yu Mi Kang, Seung Hak Lee, Byung-Mo Oh, Kyou-Sup Han, Meihua Zhang, Hoe Suk Kim, Woo Kyung Moon, Hakmo Lee, Kyong Soo Park, Hye Seung Jung
Journal of Endocrinology.2018; 239(3): 277. CrossRef - Granulocyte-colony stimulating factor as a treatment for diabetic neuropathy in rat
Kyung-Soo Kim, Yi-Sun Song, Jiyong Jin, Jun-Ho Joe, Byung-Im So, Jun-Young Park, Cheng-Hu Fang, Mi Jung Kim, Youl-Hee Cho, Sejin Hwang, Young-Suck Ro, Hyuck Kim, You-Hern Ahn, Hak-Joon Sung, Jung-Joon Sung, Sung-Hye Park, Stuart A. Lipton
Molecular and Cellular Endocrinology.2015; 414: 64. CrossRef
- Colony stimulating factors in the nervous system
- The Correlation and Accuracy of Glucose Levels between Interstitial Fluid and Venous Plasma by Continuous Glucose Monitoring System
- Young Ha Baek, Heung Yong Jin, Kyung Ae Lee, Seon Mee Kang, Woong Ji Kim, Min Gul Kim, Ji Hyun Park, Soo Wan Chae, Hong Sun Baek, Tae Sun Park
- Korean Diabetes J. 2010;34(6):350-358. Published online December 31, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.6.350
- 4,848 View
- 50 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Clinical experience with the continuous glucose monitoring systems (CGMS) is limited in Korea. The objective of this study is to evaluate the accuracy of the CGMS and the correlation between interstitial fluid and venous plasma glucose level in Korean healthy male subjects.
Methods Thirty-two subjects were served with glucose solution contained same amount of test food's carbohydrate and test foods after separate overnight fasts. CGMS was performed over 3 days during hopitalization for each subjects. Venous plasma glucose measurements were carried out during 4 hours (0, 0.25, 0.5, 0.75, 1, 2, 4 hours) just before and after glucose solution and test food load. The performance of the CGMS was evaluated by comparing its readings to those obtained at the same time by the hexokinase method using the auto biochemistry machine (Hitachi 7600-110). Also, correlations between glucose recorded with CGMS and venous plasma glucose value were examined.
Results CGMS slightly underestimated the glucose value as compared with the venous plasma glucose level (16.3 ± 22.2 mg/dL). Correlation between CGMS and venous plasma glucose values throughout sensor lifetime is 0.73 (regression analysis: slope = 1.08, intercept = 8.38 mg/dL). Sensor sensitivity can deteriorate over time, with correlations between venous blood glucose and CGMS values dropping from 0.77 during 1st day to 0.65 during 2nd and 3rd day.
Conclusion The accuracy of data provided by CGMS may be less than expected. CGMS sensor sensitivity is decreased with the passage of time. But, from this study, CGMS can be used for glucose variability tendency monitoring conveniently to the Korean.
-
Citations
Citations to this article as recorded by- Evaluation of the performance and usability of a novel continuous glucose monitoring system
Li Yan, Qiang Li, Qingbo Guan, Mingsong Han, Yu Zhao, Junfei Fang, Jiajun Zhao
International Journal of Diabetes in Developing Countries.2023; 43(4): 551. CrossRef - Correlation between short- and mid-term hemoglobin A1c and glycemic control determined by continuous glucose monitoring
Jen-Hung Huang, Yung-Kuo Lin, Ting-Wei Lee, Han-Wen Liu, Yu-Mei Chien, Yu-Chun Hsueh, Ting-I Lee, Yi-Jen Chen
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - Accuracy of Flash Glucose Monitoring During Postprandial Rest and Different Walking Conditions in Overweight or Obese Young Adults
Xiaoyuan Zhang, Fenghua Sun, Waris Wongpipit, Wendy Y. J. Huang, Stephen H. S. Wong
Frontiers in Physiology.2021;[Epub] CrossRef - The MEDGICarb-Study: Design of a multi-center randomized controlled trial to determine the differential health-promoting effects of low- and high-glycemic index Mediterranean-style eating patterns
Robert E. Bergia, Izabela Biskup, Rosalba Giacco, Giuseppina Costabile, Savanna Gray, Amy Wright, Marilena Vitale, Wayne W. Campbell, Rikard Landberg, Gabriele Riccardi
Contemporary Clinical Trials Communications.2020; 19: 100640. CrossRef - A genetic programming-based regression for extrapolating a blood glucose-dynamics model from interstitial glucose measurements and their first derivatives
I. De Falco, A. Della Cioppa, A. Giugliano, A. Marcelli, T. Koutny, M. Krcma, U. Scafuri, E. Tarantino
Applied Soft Computing.2019; 77: 316. CrossRef - Genetic Programming-based induction of a glucose-dynamics model for telemedicine
Ivanoe De Falco, Antonio Della Cioppa, Tomas Koutny, Michal Krcma, Umberto Scafuri, Ernesto Tarantino
Journal of Network and Computer Applications.2018; 119: 1. CrossRef - A high-accuracy measurement method of glucose concentration in interstitial fluid based on microdialysis
Dachao Li, Qingmei Xu, Yu Liu, Ridong Wang, Kexin Xu, Haixia Yu
Measurement Science and Technology.2017; 28(11): 115701. CrossRef - Effects of Higher Dietary Protein and Fiber Intakes at Breakfast on Postprandial Glucose, Insulin, and 24-h Interstitial Glucose in Overweight Adults
Akua Amankwaah, R. Sayer, Amy Wright, Ningning Chen, Megan McCrory, Wayne Campbell
Nutrients.2017; 9(4): 352. CrossRef - High Surface Area Electrodes Generated via Electrochemical Roughening Improve the Signaling of Electrochemical Aptamer-Based Biosensors
Netzahualcóyotl Arroyo-Currás, Karen Scida, Kyle L. Ploense, Tod E. Kippin, Kevin W. Plaxco
Analytical Chemistry.2017; 89(22): 12185. CrossRef - Hyperglycemia-Induced Changes in Hyaluronan Contribute to Impaired Skin Wound Healing in Diabetes: Review and Perspective
Sajina Shakya, Yan Wang, Judith A. Mack, Edward V. Maytin
International Journal of Cell Biology.2015; 2015: 1. CrossRef - Hypoglycemia in everyday life after gastric bypass and duodenal switch
Niclas Abrahamsson, Britt Edén Engström, Magnus Sundbom, F Anders Karlsson
European Journal of Endocrinology.2015; 173(1): 91. CrossRef - The use of reinforcement learning algorithms to meet the challenges of an artificial pancreas
Melanie K Bothe, Luke Dickens, Katrin Reichel, Arn Tellmann, Björn Ellger, Martin Westphal, Ahmed A Faisal
Expert Review of Medical Devices.2013; 10(5): 661. CrossRef - Continuous glucose monitoring: current clinical use
Hun‐Sung Kim, Jeong‐Ah Shin, Jin‐Sun Chang, Jae‐Hyoung Cho, Ho‐Young Son, Kun‐Ho Yoon
Diabetes/Metabolism Research and Reviews.2012; 28(s2): 73. CrossRef - Correlations of Glucose Levels in Interstitial Fluid Estimated by Continuous Glucose Monitoring Systems and Venous Plasma
Byung-Joon Kim
Korean Diabetes Journal.2010; 34(6): 338. CrossRef
- Evaluation of the performance and usability of a novel continuous glucose monitoring system

 KDA
KDA
 First
First Prev
Prev





